Dietitians, Cannabis, and the Education Gap No One Wants to Own
What a national survey of integrative dietitians tells us about cannabis literacy in healthcare
As cannabis use becomes increasingly normalized—medically, culturally, and commercially—patients are asking smarter, more specific questions. Unfortunately, many healthcare professionals are still being trained as if those questions don’t exist.
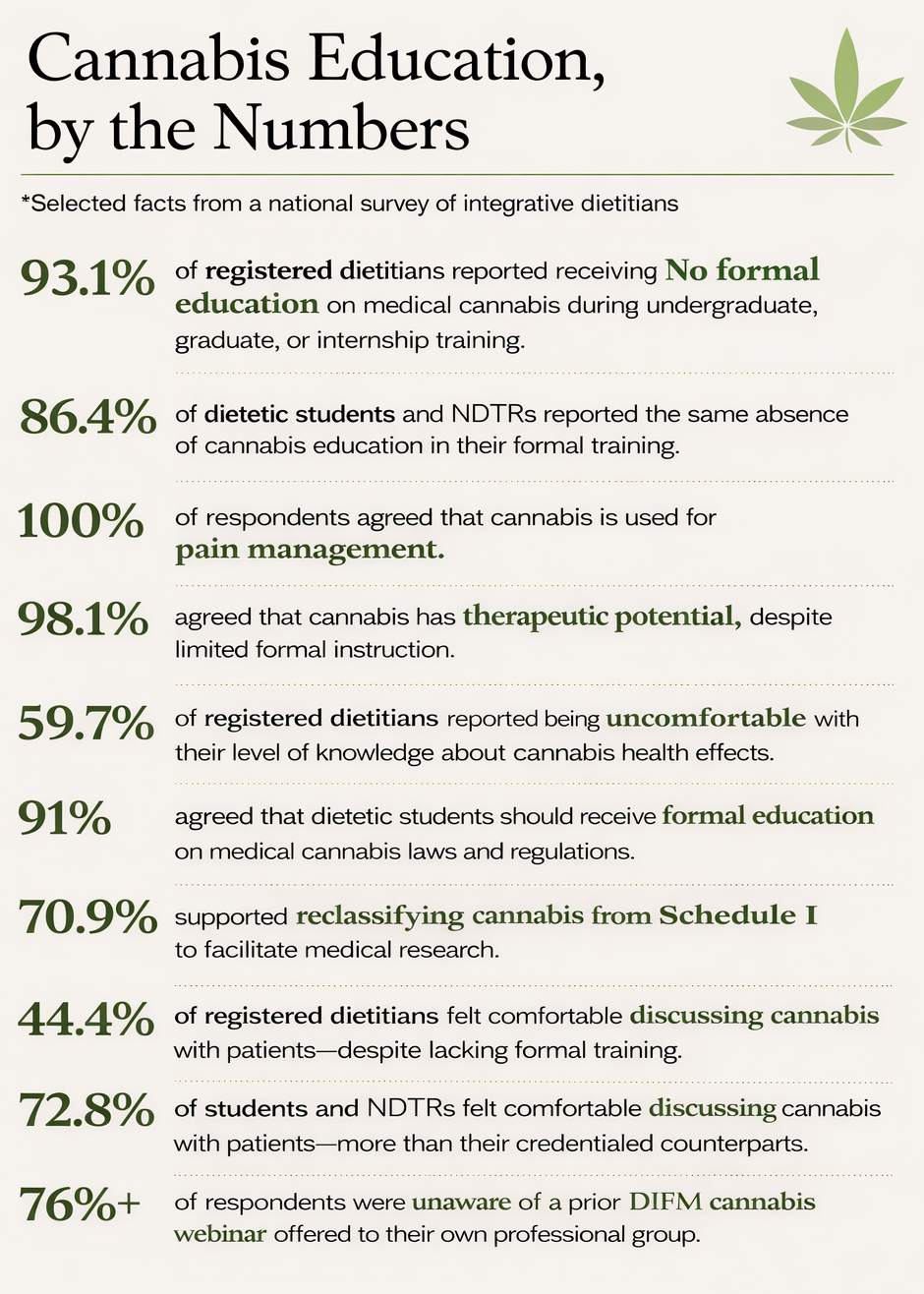
A 2023 national survey of dietitians in the Dietitians in Integrative and Functional Medicine (DIFM) practice group reveals a familiar but troubling pattern: high interest, broad acceptance of therapeutic potential, and widespread discomfort with actual knowledge. In short, clinicians know cannabis matters—but most were never taught how to talk about it.
The findings should concern anyone involved in patient education, interdisciplinary care, or professional training pipelines.
Who was surveyed—and why it matters
The study surveyed DIFM members across the United States, including registered dietitian nutritionists (RDNs), nutrition and dietetic technicians (NDTRs), and students. DIFM was an intentional choice: this group already embraces integrative, evidence-informed, and often controversial topics in clinical nutrition.
If any dietetic subgroup might be expected to feel prepared to discuss cannabis, this would be it. They weren’t.
Out of more than 3,300 eligible members, 166 completed a detailed 32-question survey assessing knowledge, attitudes, and perceptions related to cannabis education.
What dietitians agree on (almost universally)
Across credential levels, respondents showed strong agreement on several foundational points:
Cannabis has therapeutic potential, particularly for pain, appetite, and nausea
Cannabis comes in multiple delivery forms, each with different implications
State and federal cannabis laws differ, often confusing clinicians and patients alike
Cannabis carries potential risks and side effects, warranting professional guidance
These are not fringe beliefs—they represent mainstream clinical consensus.
Yet agreement on general principles did not translate into confidence.
The uncomfortable truth: “I was never trained”
The most striking finding was not skepticism—it was absence.
93.1% of RDNs reported receiving no cannabis education during undergraduate, graduate, or internship training
86.4% of students and NDTRs reported the same
A majority felt uncomfortable with their own level of knowledge about cannabis health effects
This gap persists even among clinicians practicing in states with legal medical cannabis and among professionals actively interested in integrative care.
In other words: legality and exposure do not equal education.
Willing—but hesitant—to talk with patients
Despite limited training, many respondents indicated they would discuss cannabis if necessary:
44.4% of RDNs and 72.8% of students/NDTRs felt comfortable discussing cannabis with patients or care teams
Yet fewer felt confident addressing dosing, adverse effects, or product selection
This creates a risky dynamic: clinicians are expected to engage, but without standardized knowledge, clinical guardrails, or shared language. Patients notice.
A shared expectation: someone should be teaching this
Respondents overwhelmingly agreed on several educational priorities:
Students should receive formal education on cannabis laws and clinical considerations
Physicians should receive training before recommending cannabis therapeutically
Continuing education—rather than ad hoc self-study—should be the norm
Notably, many clinicians pursued cannabis education after credentialing, suggesting demand exists—but arrives too late and too inconsistently.
Why this matters beyond dietetics
Although this study focused on dietitians, its implications extend across healthcare.
Cannabis sits at the intersection of:
pharmacology
nutrition
mental health
pain management
public health
regulation
When no profession “owns” cannabis education, patients are left navigating dispensaries, social media, and anecdote-driven advice alone.
Dietitians—particularly those trained in integrative and functional medicine—are well positioned to contribute meaningfully. But position without preparation is not enough.
What PRC+ takes from this
At PRC+, we view this study as further evidence that education must move upstream into formal curricula, structured continuing education, and interdisciplinary dialogue.
Key takeaways:
Interest is not the problem—education infrastructure is missing
Self-directed learning is insufficient for patient-facing care
Standardized, evidence-based resources remain urgently needed
Dietitians can play a leadership role—if trained appropriately
Cannabis is no longer a fringe topic. The data make clear that pretending otherwise leaves clinicians underprepared and patients underserved.
The bottom line
Patients are already using cannabis—for better or worse. The question is no longer if healthcare professionals should understand it, but who will take responsibility for teaching it properly. This study suggests dietitians are ready to engage. The system just hasn’t met them halfway yet.
PRC+ develops evidence-based cannabis and cannabinoid education for healthcare professionals, educators, regulators, and community organizations. We design and deliver custom live trainings and curriculum modules grounded in neurodevelopment, pharmacology, and public-health science. Contact PRC+ to build a training program for your institution, school, or agency. Prctrials.info@gmail.com