Why Cannabis Belongs in the Dental Hygiene Curriculum
Review of “The Need for Cannabis Education in Dental Hygiene Programs” (Joffray 2024 Journal of Dental Education 2024)
Dry Mouth, Deeper Meanings
The mouth, for all its chatter, is also a barometer of the body’s quieter systems. Cannabis, it seems, turns the faucet off at the source. By binding to cannabinoid receptors in the salivary glands, cannabinoids suppress parasympathetic activity and slow saliva production; a physiological trick that transforms a pleasant puff into a case study in xerostomia.
But dry mouth is just the beginning. The condition invites halitosis, infections, and strange eating habits, and often drives social withdrawal and stigma. As one study found, individuals living with xerostomia reported a lack of empathy and professional support, a feeling that their condition—and by extension, their cannabis use—made them outsiders. In this context, the clinical merges with the cultural: a parched mouth becomes a symptom of silence in healthcare.
And perhaps most strikingly, the very professionals who spend the most time examining mouths, dental hygienists, are the least prepared to talk about the drug that caused it.
The Stigma of Silence
For decades, hygienists have dutifully asked about tobacco and alcohol, both enshrined in every medical history form. But cannabis? That box often doesn’t exist. Even as legalization sweeps the map and dispensaries outnumber Starbucks in some cities, cannabis remains the unspoken variable in oral health.
The result is predictable: a growing population of patients managing periodontal disease, attachment loss, cavities, and oral lesions related to cannabis use, guided by clinicians who were never trained to recognize these patterns. Joffray and Johnson describe the consequences with clinical precision and quiet urgency—social withdrawal, professional discomfort, and educational neglect, all orbiting a single, solvable problem: the absence of cannabis education in dental hygiene programs.
Yet, within that absence lies possibility. The same silence that once reflected stigma now signals a readiness for reform. Hygienists are beginning to ask not if they should teach cannabis, but how.
Taking the Pulse of the Curriculum
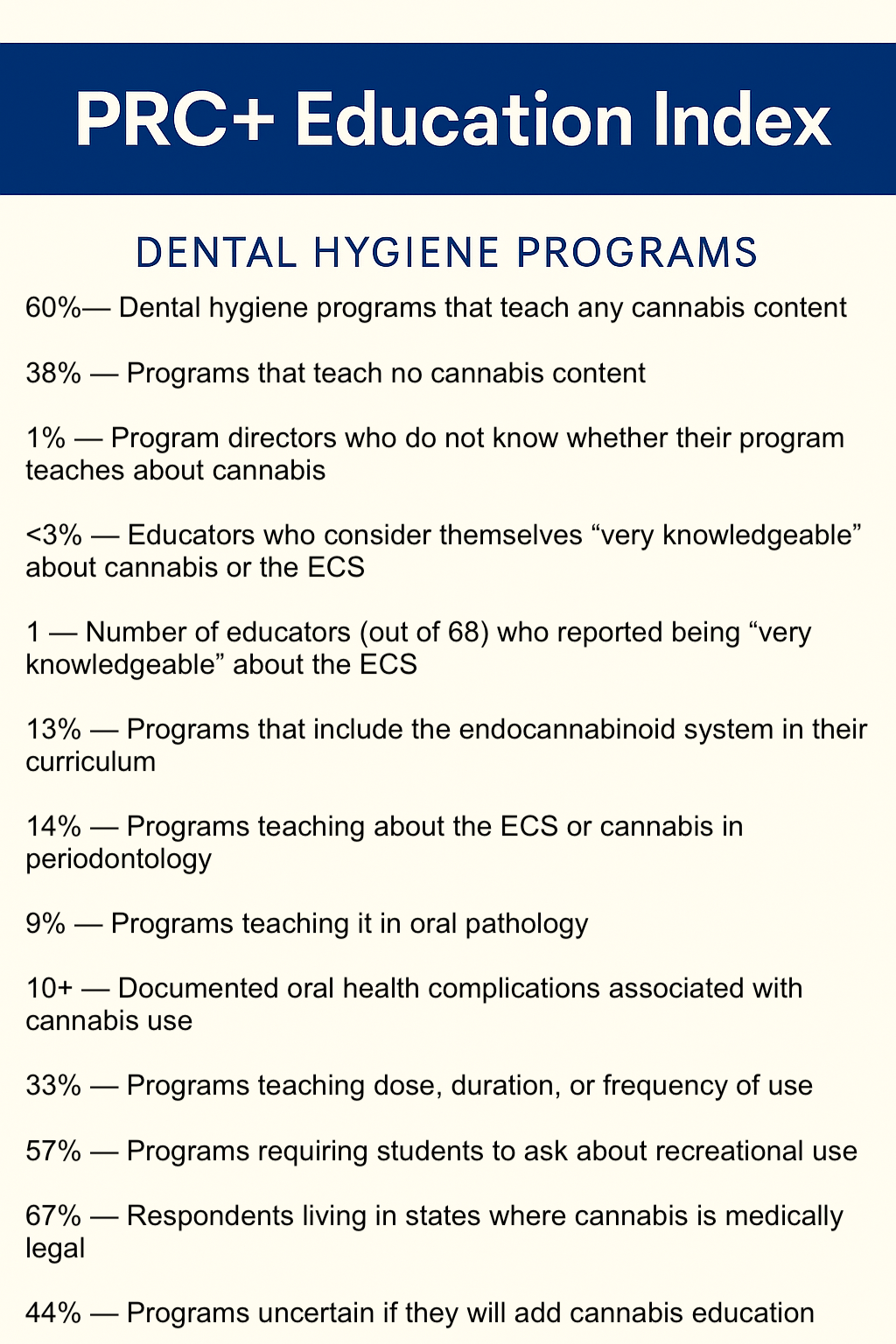
In 2021, the authors surveyed 327 dental hygiene program directors across the United States. The 26-question online instrument asked whether cannabis content was included in their curricula, where it appeared, and how legalization might influence instruction.
Only 21 percent of directors responded, though all completed the survey—a data point suggesting curiosity mixed with uncertainty rather than disinterest. Statistical analysis (chi-square tests) revealed something quietly radical: the inclusion of cannabis content had no relationship to whether a state had legalized medical cannabis. In other words, progress isn’t dictated by law but by leadership.
Brushing Without Knowledge
Of the respondents, 60 percent reported teaching some cannabis-related content, while 38 percent did not. Even where it was taught, the material was often superficial—most frequently tucked into pharmacology lectures (50 percent) or clinical seminars (41 percent), with only 13 percent addressing the endocannabinoid system (ECS) itself.
Less than 3 percent of educators felt “very knowledgeable” about cannabis or the ECS. The study found no statistically significant difference between states where cannabis was legal and those where it wasn’t. The authors summarize the paradox neatly: legality has changed faster than literacy.
It’s a bit like teaching oral hygiene without mentioning teeth.
Voices from the Clinic Floor
These statements—simple, declarative, and direct—read less like conclusions and more like mandates. The authors argue that cannabis education should be standard practice, as essential to oral health as fluoride or radiographs.
Why the Mouth Matters in the Cannabis Conversation
Cannabis use isn’t only a social or pharmacological issue; it’s a biological one, written in the tissues of the mouth. Regular use is linked to xerostomia, halitosis, periodontal disease, delayed healing after surgery, and even premalignant lesions. The mechanism is well-documented: cannabinoids reduce saliva, alter immune signaling, and influence vascular tone.
When hygienists fail to ask about cannabis use, they miss opportunities to catch and counsel on these early signs. The omission isn’t neutral—it’s clinical blindness. As legalization expands, understanding cannabis’s impact on oral health becomes not an elective skill but a professional obligation.
Lessons from the Hygienist’s Chair
For educators and practitioners alike, this study offers a clear set of lessons:
Ask every patient about cannabis use, just as routinely as tobacco or alcohol.
Include ECS fundamentals in biomedical and pharmacology coursework.
Teach students to counsel with curiosity, not judgment—stigma silences disclosure.
Address adverse oral effects: hydration, saliva substitutes, fluoride use, and shorter recall intervals.
Develop standardized assessment forms with checkboxes for cannabis use and guidance on oral-care interventions.
In short: if you don’t teach it, you can’t treat it.
Connecting the Dots: From Policy to Practice
The absence of cannabis education across healthcare isn’t due to a lack of evidence—it’s due to inertia. Medicine, dentistry, and public health have long been reactive fields, expanding curricula only after the public has already moved on.
Tobacco and alcohol education became staples only after decades of morbidity and litigation. Cannabis now stands at that same threshold. Joffray and Johnson’s data make a quiet but unmistakable point: whether legal or not, cannabis is already in your clinic. The question is whether your staff knows what to do about it.
Polishing the Future
Education, like enamel, erodes when ignored. This study reminds us that the legalization wave isn’t just a legal or economic event—it’s a clinical one. The public’s habits have changed; their healthcare must follow.
A hygienist trained to ask about cannabis use isn’t being provocative; they’re being responsible. For a profession rooted in prevention, acknowledging cannabis’s place in oral health is not radical—it’s overdue.
PRC+ Note
At PRC+, we create custom educational modules and continuing education programs on cannabis and cannabinoid science for clinicians, educators, and allied health professionals.
Reach out to our team to develop accredited or non-accredited content for your institution—bridging knowledge gaps, reducing stigma, and equipping practitioners to meet patients where they are.
Contact us: Prctrials.info@gmail.com