Medical Cannabis Across Borders: What Physicians Really Know (and Don’t)
Cannabis has quietly achieved global citizenship. As of 2023, over 40 countries permit some form of medical use, and yet the physicians entrusted to guide patients are often left with patchy maps and shifting rules. Syed and colleagues (2023) sought to chart this terrain by surveying 323 physicians from 17 countries, including the U.S., Egypt, Croatia, India, Portugal, and Turkey. Their findings capture the international ambivalence: curiosity, caution, and an urgent call for education.
The Study at a Glance
Sample: 323 physicians (mean age ~35 years; 53% women; average 10 years’ practice experience).
Countries: 17, spanning North America, Europe, Asia, Africa, and the Middle East.
Design: A 28-question survey probing physician demographics, knowledge, attitudes, and willingness to recommend cannabis in case scenarios.
Source: Syed 2023
What the Data Showed
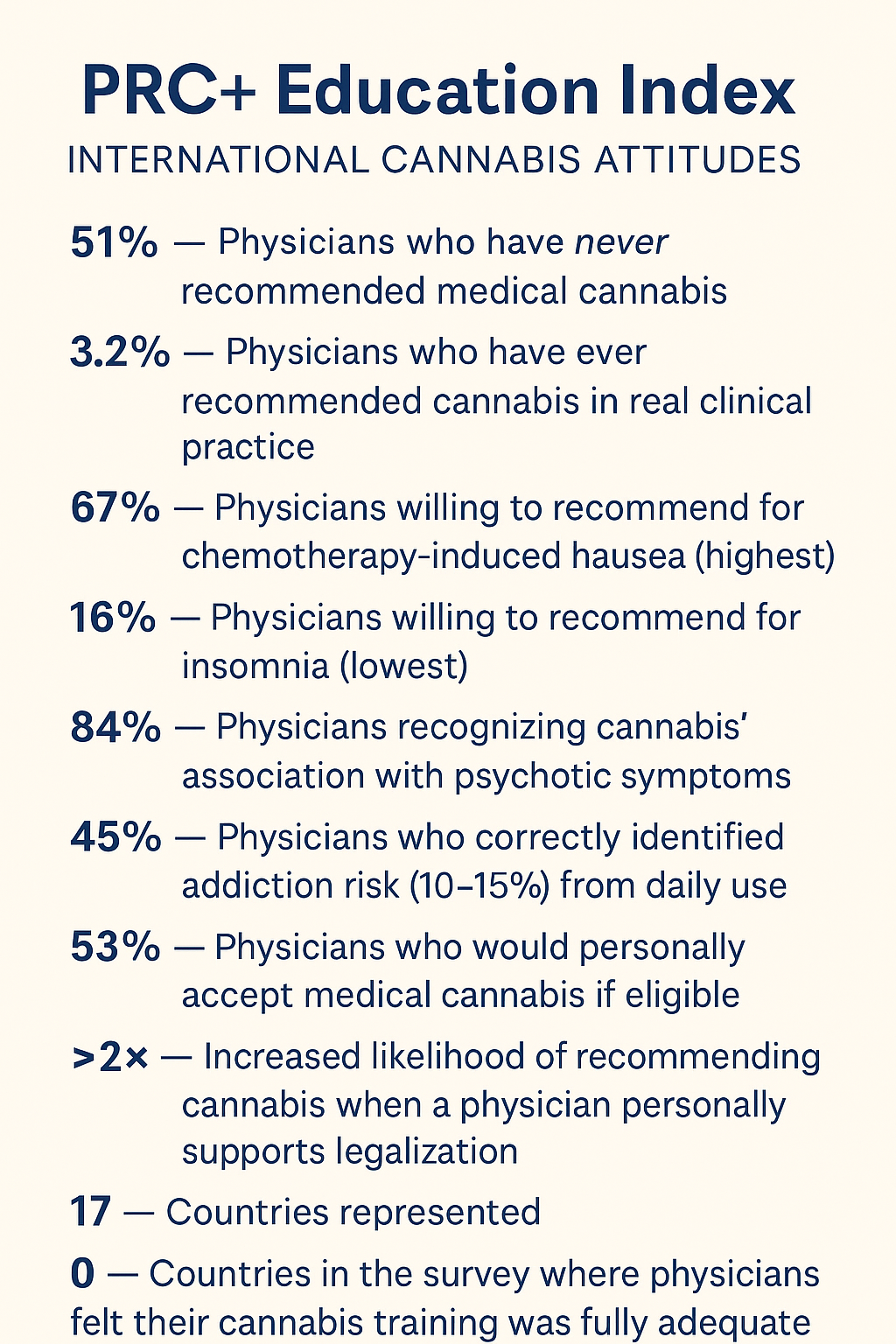
Minimal prescribing experience. Over half (51.4%) had never recommended cannabis but were open to it; 33% admitted they “did not know enough”; only 3.2% reported any real prescribing experience
Knowledge gaps. When asked about cannabis addiction risk with daily use, only 45% answered correctly (10–15%). Nearly one in five underestimated risk (<1%), while 13% overestimated it (>50%)
Psychosis recognition. Encouragingly, 84% acknowledged the association between cannabis use and psychotic symptoms, based on clinical experience
Willingness varies by condition. Highest for chemotherapy-induced nausea (67%), refractory neuropathic pain (52%), and ALS-related spasticity (52%). Lowest for insomnia (16%), cirrhosis with alcohol use disorder (19%), and autism with self-injury (22%)
Personal beliefs matter. About half (53%) said they would accept cannabis themselves if eligible. Physicians holding favorable personal beliefs were significantly more likely to recommend cannabis for patients — even when evidence or guidelines discouraged it
As the authors conclude:
“Medical decisions related to cannabis are guided as much by personal beliefs as by scientific evidence. This highlights the urgent need for domain-specific education and clearer guidelines.”
Global Clusters of Cannabis Views: How Physicians Line Up Across Borders
One of the most compelling insights from the Syed et al. (2023) international survey isn’t just what individual physicians think about medical cannabis — it’s how their views cluster by geography, culture, and comfort level. When the responses are grouped, four clear profiles emerge. These clusters show that cannabis conversations may be global, but the readiness to engage in them is anything but uniform.
Cluster 1: Evidence-Aligned & Moderately Supportive
(Portugal, United States, Croatia)
These countries form the “evidence-friendly middle,” where physicians show a reasonable willingness to recommend cannabis for conditions with solid support, such as chemotherapy-induced nausea or ALS-related spasticity. Confidence levels vary, but their practice patterns tend to mirror clinical evidence more than personal ideology.
Cluster 2: Interested but Undertrained
(India, Egypt)
Here the interest is palpable, the curiosity real — but formal training is scarce. Physicians in these countries often recognize psychosis-related risks and express openness to medical use, yet many cite insufficient knowledge as the key barrier to recommending cannabis.
Cluster 3: Highly Cautious / Limited Support
(Turkey and neighboring Middle Eastern respondents)
This cluster reflects the most conservative stance. Confidence in cannabis knowledge is low, willingness to recommend is lower, and decisions are shaped predominantly by legal and cultural constraints. Caution outweighs curiosity in nearly every domain.
Cluster 4: Values-Driven Decision Makers
(Spread across Europe, South America, and Asia)
These physicians don’t align by geography but by mindset. Their willingness to recommend cannabis tracks more closely with personal beliefs than with guidelines. When they favor cannabis legalization, their recommendations surge — even in clinical scenarios where evidence is limited. When skeptical, recommendations flatline, regardless of evidence.
Across all four clusters, one truth holds: training remains the universal missing ingredient. Whether in Portugal or Punjab, understanding cannabis relies less on proximity to legalization and more on access to high-quality education.
Why This Matters
The survey reveals not just gaps in knowledge, but inconsistencies between evidence, guidelines, and practice. For example, many physicians were willing to recommend cannabis for PTSD or autism — conditions where major medical societies caution against it. Conversely, only about half aligned with guidelines that do support cannabis for severe spasticity in MS or ALS.
In whimsical terms: cannabis remains a test question where too many physicians are still filling in the bubbles based on gut instinct rather than the answer key.
Lessons for Healthcare Professionals
Evidence ≠ Belief. Physician recommendations often reflected personal attitudes rather than guidelines.
Addiction awareness is uneven. Underestimating or overestimating risk alike leads to poor clinical guidance.
Global variation persists. Cultural, political, and regulatory climates shape physician willingness as much as evidence.
Training is universal need. Regardless of geography, structured cannabis education remains the missing ingredient.
Connecting the Dots
Placed alongside the Weisman & Rodríguez (2021) systematic review, Worster et al. (2023) interprofessional clinician survey, and Cronin et al. (2025) training intervention, the Syed et al. study supplies a global layer. Across decades, disciplines, and borders, the refrain is the same: physicians are willing, patients are asking, but education and evidence must catch up.
Closing Thought
The international perspective makes one thing clear: cannabis is no longer a fringe issue. Whether in Cairo or Connecticut, patients expect informed conversations. For physicians, the choice is not whether cannabis will come up — it’s whether they’ll be ready for the discussion.
PRC+ offers training modules and develops high-quality educational programs on cannabis and cannabinoids. Whether your focus is clinical practice, public health, or research, our team can design evidence-based training tailored to your needs. Reach out to us today to create a custom live training, conducted and instructed by our team of experts. Prctrials.info@gmail.com