Older Adults, Cannabis, and the Quiet Gap in Clinical Conversations
What a Philadelphia Pilot Study Tells Us—and What It Asks of Clinicians
Cannabis use among adults aged 65 and older is no longer an edge case—it is a growing clinical reality. Yet, as legalization advances and older adults increasingly view Cannabis as a legitimate therapeutic option, the healthcare system appears to be lagging behind in one critical area: routine, evidence-based conversations between patients and clinicians.
A 2023 pilot study published in the Journal of Primary Care & Community Health explored attitudes, beliefs, and perceptions about Cannabis among adults aged 65 and older living in Philadelphia. The findings offer a revealing snapshot of how older adults think about Cannabis—and where clinical practice may be falling short.
What Older Adults Believe—and What They Don’t
Among the 47 participants surveyed (average age: 71 years):
76% considered cannabis a highly important treatment option for older adults
79% reported feeling comfortable discussing Cannabis with their primary care provider
98% believed physicians should offer Cannabis as a treatment option for conditions common in older age
At the same time, notable knowledge gaps emerged. Many participants were uncertain about:
Drug–drug interactions (particularly with cardiovascular, metabolic, and psychiatric medications)
Long-term effects
Adverse events and safest routes of administration
This combination of high confidence paired with incomplete risk awareness is a familiar phenomenon in emerging therapeutic spaces. The authors describe it as a form of overclaiming: believing one knows more than one actually does. In Cannabis medicine, this gap can have real clinical consequences.
The Missed Moment in Primary Care
Perhaps the most clinically actionable finding is also the most concerning:
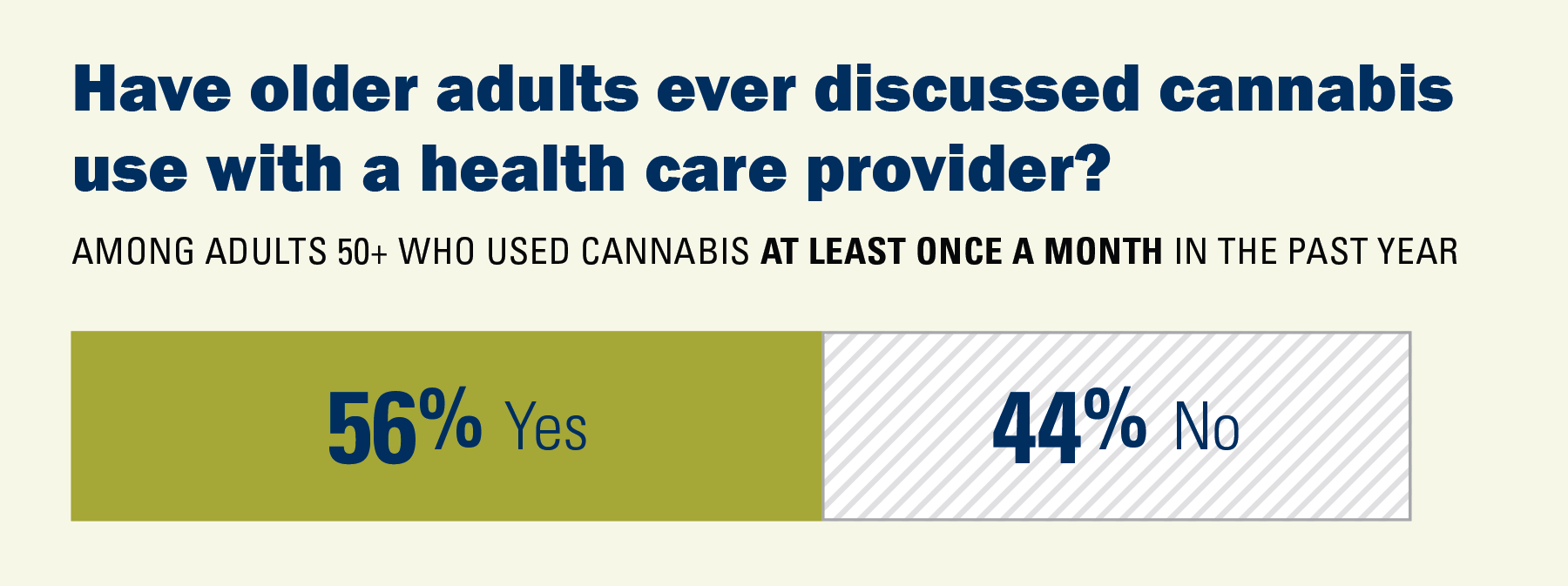
Only 23% of participants reported being asked about cannabis use by their primary care provider
By comparison, 55–57% were asked about tobacco or alcohol use
This is despite the fact that most participants said they were comfortable having the discussion—and believed it belonged in routine care.
In other words, patients are ready, but clinicians are not consistently initiating the conversation.
Where Patients Are Getting Their Information
When clinicians don’t lead, other sources fill the vacuum:
The internet and social media were the most common sources of cannabis information
Friends and family ranked higher than healthcare providers
Only a small minority cited their PCP as a primary source of cannabis guidance
This mirrors broader trends seen in public-health research: patients increasingly rely on non-clinical sources for cannabinoid information, even when medical complexity is high.
Why This Matters for Clinical Practice
Older adults are more likely to:
Take multiple prescription medications
Experience altered pharmacokinetics and pharmacodynamics
Face higher risks from sedation, falls, and cognitive impairment
Cannabis does not exist outside this reality—it interacts with it.
The study’s findings underscore a growing need for:
Clinician education on cannabis pharmacology, interactions, and risk assessment
Standardized screening for Cannabis use alongside alcohol and tobacco
Clear, evidence-based counseling frameworks tailored to older adults
Importantly, this is not a call for advocacy or avoidance—it is a call for clinical competence.
The Takeaway for PRC+ Clinicians and Researchers
This pilot study highlights a simple but urgent truth:
Cannabis has entered geriatric care—but not yet on clinical terms.
Older adults are open to discussion. They see potential benefit. They want physician involvement. What remains unclear is whether the healthcare system is prepared to meet that demand with the same rigor applied to other therapeutics.
For clinicians, researchers, and educators, the next step is not debate—it is translation: turning emerging evidence into practical, patient-centered guidance that acknowledges both promise and risk.
At PRC+, this is where education, research design, and clinical insight intersect—and where the next generation of Cannabis-informed care must be built.
Related PRC+ Reading
AGE, EDUCATION, AND COMPETENCY: WHAT MEDICAL CANNABIS PATIENTS IN ISRAEL TEACH US ABOUT PHYSICIAN TRAINING
WHY CANNABIS BELONGS IN THE DENTAL HYGIENE CURRICULUM
“IT’S LEGAL, NOW WHAT?” A REVIEW OF INTERDISCIPLINARY CANNABIS TRAINING FOR HEALTHCARE PROFESSIONALS
PRC+ ENDNOTE
PRC+ develops evidence-based cannabis and cannabinoid education for healthcare professionals, educators, regulators, and community organizations. We design and deliver custom live trainings and curriculum modules grounded in neurodevelopment, pharmacology, and public-health science. Contact PRC+ to build a training program for your institution, school, or agency. Prctrials.info@gmail.com